059
CHAPTER 7
Polio Infantile Paralysis
HOW TO RECOGNIZE PARALYSIS CAUSED BY POLIO
 | Intelligence and the mind are not affected. |
 | Feeling is not affected. |
 | 'Knee jerks' and other tendon reflexes in the affected
limb are reduced or absent. (In cerebral palsy, 'knee jerks' often
jump more than normal. See Page 88.)
Also, the paralysis of polio is 'floppy'; limbs affected by cerebral
palsy often are tense and resist when straightened or bent (see
Page 102). |
|
 |
 | The paralysis does not get worse with time. However, secondary
problems like contractures, curve of the backbone and dislocations may
occur.
|
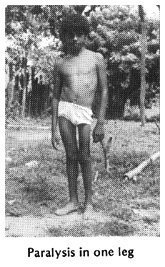
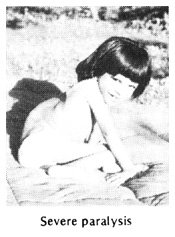
| Of children who become paralyzed by polio: |
 30%
recover completely in the first weeks or months. 30%
recover completely in the first weeks or months. |
 30%
have mild paralysis. 30%
have mild paralysis. |
 30%
have moderate or severe paralysis. 30%
have moderate or severe paralysis. |

10% die (often because of difficulty breathing or swallowing). |
060
BASIC QUESTIONS AND ANSWERS ABOUT POLIO
How common is it? In many countries, polio - or
'poliomyelitis'- is still the most common cause of physical disability in
children. In some areas, at least one of every 100 children may have some
paralysis from polio. Where vaccination programs are effective, polio has
been greatly reduced.
What causes it?A virus (infection). The
infection attacks parts of the spinal cord, where it damages only the
nerves that control movement. In areas with poor hygiene and lack of
latrines, the polio infection spreads when the stool (shit) of a sick
child reaches the mouth of a healthy child. Where sanitation is better,
polio spreads mostly through coughing and sneezing.
Do all children who become infected with the polio virus become
paralyzed? No, only a small percentage become paralyzed. Most
only get what looks like a bad cold, with fever. However, if a child with
a 'cold' caused by the polio virus is given an injection of any
medication, the irritation caused by the injection can
bring on paralysis. (See warning on Page
19.)
Is the paralysis contagious? No, not after 2 weeks
from when a child first gets sick with polio. In fact, most polio is
spread through the stool of non-paralyzed
children who have 'only a cold' caused by the polio virus.
At what age do children get polio? In areas with poor
sanitation, polio most often attacks babies from 8 to 24 months
old, but occasionally children up to age 4 or 5. As sanitation improves,
polio tends to strike older children and even young adults.
Who does it most often affect? Boys, a little more
than girls. Unvaccinated children much more often than vaccinated
children. (See Page 74). Young children who are given
injections unnecessarily are paralyzed by polio more often those who are
not.
How does the paralysis begin? It begins after signs of
a cold and fever, sometimes with diarrhea or vomiting. After a few days
the neck becomes stiff and painful and parts of the body become limp.
Parents may notice the weakness right away, or only after the child
recovers from the acute illness.
Once a child is paralyzed, what changes or improvements can be
expected? Often the paralysis will gradually go away, partly or
completely. Any paralysis left after 7 months is usually permanent. The
paralysis will not get worse. However, certain secondary problems may
develop-especially if precautions are not taken to prevent them.
What are the child's chances of leading a happy, productive
life? Usually very good-provided the child is encouraged to do
things for himself, to get the most out of school, and to learn useful
skills within his physical limitations (see Page
497).
Can persons with polio marry and have normal children?
Yes. Polio is not inherited (familial) and does not affect ability to have
children.
061
SECONDARY PROBLEMS TO LOOK FOR WITH POLIO
By secondary problems, we mean further disabilities or
complications that can appear after, and because of, the original
disability.
CONTRACTURES OF JOINTS
| A contracture is a shortening of muscles and tendons
(cords) so that the full range of limb movement is prevented. Unless
preventive steps are taken, joint contractures will form in many
paralyzed children. Once formed, often they must be corrected before
braces can be fitted and walking is possible. Correction of advanced
contractures, whether through exercises, casts, or surgery (or a
combination), is costly, takes time and causes discomfort. Therefore
early prevention of contractures is very important.
A full discussion of contractures, their causes, prevention, and
treatment is in the next chapter (Chapter
8). Methods and aids for correcting contractures are described in
Chapter 59. |
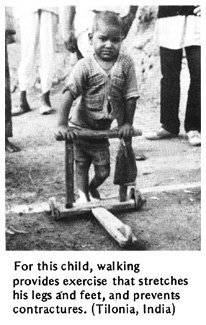
| TYPICAL CONTRACTURES IN POLIO
A child with paralysis who crawls
around like this rid never straightens her legs will gradually develop
contractures so that her hips, knees, and ankles can no longer be
straightened.
|
 |
OTHER COMMON DEFORMITIES
Weight bearing (supporting the body's weight) on weak joints can cause
deformities, Including:
| OVER-STRETCHED
JOINTS |
DISLOCATIONS
|

|
WARNING:
Dislocations like these are sometimes caused by
stretching contractures incorrectly. (See
Page 28.) |
|
 SPINAL
CURVE SPINAL
CURVE
Minor curve of spine can be caused by tilted hips, as
a result of a short leg.
More serious curve of the spine is caused by muscle weakness of the
back or body muscles. The curve can become so severe that it endangers
life by leaving too little room for the lungs and heart. |
 At
first, the spinal curve straightens when the child is positioned
better. But in time the curve becomes more fixed (will not straighten
any more). For information on spinal curves, see
Chapter 20. At
first, the spinal curve straightens when the child is positioned
better. But in time the curve becomes more fixed (will not straighten
any more). For information on spinal curves, see
Chapter 20. |
062
WHAT OTHER DISABILITIES CAN BE CONFUSED WITH POLIO?
 | Sometimes cerebral palsy can be mistaken for
polio-especially cerebral palsy of the 'floppy' type. |
| However, cerebral palsy
usually affects the body in typical patterns:
 |
Polio has a more
irregular pattern of paralysis.  |
In cerebral palsy, usually you can find other signs of brain damage:
over-active knee jerks and abnormal reflexes (see
Page 88), developmental delay, awkward or uncontrolled movement, or
at least some muscle tenseness (spasticity).

 | In muscular dystrophy, paralysis begins little by
little and steadily gets worse (see Page 109). |

 | Hip problems (see Page 155)
can cause limping, and muscles may become thin and weak. Check hips for
pain or dislocations. (Note: Dislocated hip may also occur secondary to
polio.) |
| Note: Polio can occur before or after a child
has any of these other problems. Check carefully. |


 | 'Erb's palsy', or partial paralysis in one arm and
hand, comes from birth injury to the shoulder (see
Page 127). |

 | Leprosy. Foot and hand paralysis begins gradually
in older child. Often there are skin patches and loss of feeling (see
Page 215). |

 | Spina bifida is present from birth. There is
reduced feeling in the feet, and often a lump (or scar from surgery) on
the back (see Page 167). |
| ALWAYS EXAMINE THE BACK IN A CHILD WITH PARALYSIS OF THE LEGS, AND
CHECK FOR FEELING. |

 | Injuries to the spinal cord (see
Page 175) or to particular nerves going to the arms or legs. There
is usually a history of a severe back or neck injury, and loss of
feeling in the paralyzed part. |

 | Tuberculosis of the spine can cause gradual or
suddenly increasing paralysis of the lower body. Look for typical bump
on spine (see Page 165).
|
 | Other causes of paralysis or muscle weakness. There
are many causes of floppy paralysis similar to polio. One of the most
common is 'Guillain-Barre' paralysis. This can result
from a virus infection, from poisoning, or from unknown causes. It
usually begins without warning in the legs, and may spread within a few
days to paralyze the whole body. Sometimes feeling is also reduced.
Usually strength slowly returns, partly or completely, in several weeks
or months. Rehabilitation and prevention of secondary problems
are basically the same as for polio. |
063
WHAT CAN BE DONE?
DURING THE ORIGINAL ILLNESS, when the child first
becomes paralyzed:
 | No medicines help, either during the first
illness, or later. |
 | Rest is important. Avoid forceful exercise
because this may increase paralysis. Avoid injections. |
 | Good food during recovery helps the child become
stronger. (But take care that the child does not eat too much and get
fat. An overweight child will have more problems with walking and
other movements.) For suggestions about good food, see
Where There Is No Doctor,
Chapter 11. |
 | Position the child to be comfortable and to avoid
contractures. At first the muscles will be painful, and the child will
not want to straighten his joints. Slowly and gently try to straighten
his arms and legs so that the child lies in asgood a position as
possible. (See Chapter 8.) |
| GOOD POSITION

Arms, hips, and legs as straight as possible. Feet supported. |
BAD POSITION

Bent arms, hips, and legs. Feet in tiptoe position. |
Note: To reduce pain, you may need to put
cushions under the knees, but try to keep the knees as straight as you
can.
FOLLOWING THE ORIGINAL ILLNESS:
 | Continue with good food and good
positions. |
 | As soon as the fever drops, start exercises to
prevent contractures and return strength. Range-of-motion
exercises are described in
Chapter 42. Whenever possible, make exercises fun. Active
games, swimming, and other activities to keep limbs
moving as much as they can are important throughout the
child's rehabilitation. |
 |
Crutches, leg braces(calipers), and other
aids may help the child to move better and may prevent contractures or
deformities. |
 | In special cases, surgery may be needed to
correct contractures, or to change the place where strong muscles
attach, so that they help do the work of weak ones. When a foot is
very floppy or bends to one side, surgery to join certain bones of the
foot may help. But because bone surgery stops the growth of the foot,
usually it should not be done before age 12 or 13. |
 | Encourage the child to use his body and mind as
much as possible, to play actively with other children, to
take care of his daily needs, to help with work,
and to go to school. As much as possible,
treat him like any other child. |
064
REHABILITATION OF THE CHILD WITH PARALYSIS
All children paralyzed by polio can be helped by certain basic
rehabilitation measures-such as exercise to keep a full range of motion
in the affected limbs.
However, each child will have a different combination and
severity of paralyzed muscles, and therefore will have his own special
needs.
For some children, normal exercise and play may be all that are
needed. Others may require special exercises and playthings. Still
others may need braces or other aids to help them move about better, do
things more easily, or keep their bodies in healthier, more useful
positions. Those who are severely paralyzed may be helped most by a
wheelboard (trolley) or wheelchair.
Every child needs to be carefully examined and evaluated in
order to best meet his or her particular needs. The earlier you evaluate
a child's needs, and take steps to meet them, the better.
Unfortunately, 'in most areas where polio is still common, village
rehabilitation programs do not exist or are just beginning. Many
children (and adults) who have been paralyzed for a long time already
have severe deformities or joint contractures. Often these must be
corrected before a child can use braces or begin to walk.
Because contractures are such a common problem, not only with polio
but with many other disabilities, we discuss them separately in the next
chapter. Before evaluating a child with polio, we strongly
suggest you read Chapter 8 on
contractures.
| WARNING: Before deciding on any aid or
procedure, carefully consider its advantages and disadvantages. For
example, some deformities may be best left uncorrected because they
actually help the paralyzed child stand straighter or walk better (see
Page 530). And some aids or braces may prevent a child from
developing strength to walk without aids (see
Page 526).Before deciding what aid or procedure to use,
we suggest you read Chapter 56,
"Making Sure Aids and Procedures Do More Good Than Harm." |
065
PROGRESS OF A CHILD WITH POLIO:
THE CHANGING NEEDS FOR AIDS AND ASSISTANCE

1. exercises to keep full range of motion, starting
within days after paralysis appears and continuing throughout
rehabilitation

2. supported sitting in positions that help prevent
contractures

3. active exercises with limbs supported, to gain
strength and maintain full motion
4. exercise in water - walking, floating, and swimming, with
the weight of the limbs supported by the water

5. wheelboard or wheelchair with supports to prevent
or correct early contractures.

Note: These also provide good arm exercise
in preparation for walking with crutches.

6. braces to prevent contractures and prepare for
walking

7. parallel bars for beginning to balance and walk

8. walking machine or 'walker'

9. crutches modified as walker for balance and extra
support

10. under arm crutches

11 . forearm crutches and perhaps in time . . .

12. a cane or no arm supports at all
Note: These pictures are only an example -
but most of the steps are necessary for many children. Children who
begin rehabilitation late may also have contractures or deformities
requiring corrective steps not shown here.
066
EVALUATING A CHILD'S NEEDS FOR AIDS AND PROCEDURES
Step 1: Start by learning what you can through
talking with the child and family (see Child's History,
Page 37 to 38). As you do this,
watch the child move about. Observe carefully which parts of
the body seem strong, and which seem weak. Look for any differences
between one side of the body and the other-such as differences in the
length or thickness of the legs. Are there any obvious deformities, or
joints that do not seem to straighten all the way? If the child walks,
what is unusual about the way she does it? Does she dip forward or to
one side? Does she help support one leg with her hand? Is one hip lower
than the other? Or one shoulder? Does she have a humpback, a swayback,
or a sideways curve of the back?
These early observations will help you know what parts of the body
you most need to check for strength and range of motion. Often, by
watching a child you can begin to get an idea about what kind of aids or
assistance may help. For example:

Carmen appears to have severe paralysis affecting both legs and
her right arm. Weakness in her trunk (main part of the body) appears
to have caused a severe S-shaped curve of the spine. |

She will probably never walk, and will need a wheelchair or
wheelboard.
You may want also to make her a body brace, or help her in other
ways to sit more upright and try to keep the spine from bending
more. |

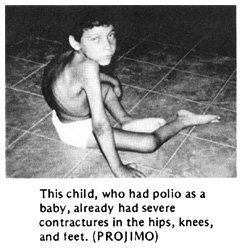
Pedro appears to have severe paralysis in his legs and hips. It
looks as if his hips, knees, and feet cannot straighten
(contractures). Weak stomach muscles and severe hip contractures may
be the cause of his swayback.
Because his arms look strong, Pedro will probably be able to walk
with crutches and leg braces. But first his contractures must be
straightened.
If the contractures cannot be straightened by gradual stretching,
he may need surgery. |
067
Manuel walks with the help of a stick. He appears to have
paralysis mainly in his right leg and foot. Because of weak thigh
muscles, he 'locks' his knee backward in order to bear weight on
it. This 'back-kneeing' has become more and more extreme as the
cords behind the knee stretch. The foot is very unstable and flops
to one side. The weaker leg looks somewhat shorter-and for walking
is much shorter because of the bent-back knee and bent-over foot.

He might be able to walk without the stick if he uses a
below-knee brace to stabilize his foot. (See
Page 550.)
But the back-knee would become worse and worse until he could
not walk. So probably he should have a long-leg brace. The brace
might allow his knee to bend backward just a little for stability
- so that no knee lock is needed. |

Afia leans forward and pushes her weak left thigh with her
hand when she walks. Her left knee cannot quite straighten. Her
weak leg looks a little shorter than the other.
Exercises to get her knee straighter or so it can bend very
slightly backward may be all that is needed for Afia to walk
without using her hand.

Or she may need an above-knee brace with a strap to pull the
knee back.
Or she may only need a below-knee brace that helps push her
knee back.
The brace bends the foot down just a little, so that by
bearing weight on toes (rather than heel) her knee is pushed
back.
To get a better idea about which of the three solutions may
work best for Afia, you will need to do a careful physical
examination, testing range of motion and muscle strength of the
hip, knee, and ankle joints. |
Step. 2: This is the physical
examination. It should usually include:
1.Range-of-motion testing, especially where
you think there might be contractures. (See "Physical
Examination," Page 27 to 29, and
"Contractures," Page 79 and
80.)
2. Muscle testing, especially of muscles
that you think may be weak. Also test muscles that need to be
strong to make up for weak ones (such as arm and shoulder
strength for crutch use). (See Page 27
and Page 30 to 33.)
3. Check for deformities: contractures;
dislocations (hip, knee, foot, shoulder, elbow); difference in
leg length; tilt of hips; and curve or abnormal shape of the
back. (See Page 34.)
068
Step 3: After the physical exam,
again observe how the child moves or walks. Try to
relate her particular way of moving and walking with
your physical findings (such as weakness of certain
muscles, contractures, and leg length). (For an example,
see Page 70.)
Step 4: Based on your observations and
tests, try to figure out what kind of exercises, aids,
or assistance might help the child most. Consider the
advantages of different possibilities: benefit, cost, comfort,
appearance, availability of materials, and whether the child is
likely to use the aid you make. Ask the child and parents for
their opinions and suggestions.
Step 5: Before making a final brace or aid
to fit the child, if possible test to see how well it
may work by using a temporary aid or old brace from
another child. For example,
If a child's ankle bends over to the outside like this... |

...a lift on the outer side of the sole like this, may
help to keep the foot straighter. |
But before nailing and glueing in the lift, quickly make
a trial one of cardboard or something else and fasten it
temporarily to the sandal or shoe with tape or string. Then
have the child walk.
Note: For a few children, a
lift like this will help. For many it will not. |
| Ask the child what she thinks.
|
Step 6: After the child, her parents, and
you have decided what kind of brace or aid might work best,
take the necessary measurements and make the brace or
aid. When making it, once again it is wise to put it
together temporarily so that you can make adjustments before
you rivet, glue, or nail it into its final form. (See
Page 540.)
Step 7: Have the child try the
brace or aid for a few days to get used to it and to
see how well it works. Ask the child and parents if it seems
to help. Does it hurt? Are there any problems? How could it be
improved? Is there something that might work better? Make what
adjustments are necessary. But remember that no brace or aid
is likely to meet the needs of a child perfectly. Do the best
you can.
069
Here is a story of how workers in a small village
rehabilitation program figured out what kind of aids a child
needed. How many of the steps we have just discussed
did they follow? Was each step important?
A STORY: A BRACE FOR SAUL
One day a mother from a neighboring village arrived at the
village center with her 6 year old son, Saul. Mari and Chelo,
2 of the village rehabilitation workers, welcomed them warmly.
Learning that Saul had polio as a baby, they asked him to
walk, and then to run, while they watched carefully. Saul
limped a lot and one leg looked thinner and shorter. With each
step it bent back at the knee.
"He walks quite well, really," said Mari. "But he has to
'lock' his knee back in order to put weight on it. That knee
is going to keep stretching back and some day it will give
out."
"A long-leg brace would protect his knee," suggested Chelo.
"Oh, please, no!" said Saul's mother. "A year ago we took
Saul to the city and the doctors had a big metal brace made
for him. It cost so much we are still in debt! Saul hated it!
He would always take it off and hide it. We tried and tried to
get him to use it, but he wouldn't."

"That's not surprising," said Mari. "Often a child who can
walk without a brace will refuse to use one-even if he walks
better with it. We could make him a long-leg brace out of
plastic. It would be much lighter. What do you say, Saul?"
Saul began to cry.
"Don't worry, Saul. Maybe we can do something simpler,"
said Mari. "But first let's examine you, okay?" Saul nodded.
On muscle testing Saul, they found he could not straighten
his knee at all. But he had fair strength for bending his knee
back

and his hip forward,
and good strength for bending his hip back.
070
"With the hip and thigh strength he has, he should almost
be able to stand on that leg without the knee bending back,"
said Mari. "Saul, let's see you try it like this. Pretend
you're a stork!" For a moment Saul could do it. "Good!" said
Mari. "Every day stand like that and see how high you can
count without letting your knee go back. Every day try to beat
your old record! Okay?"
"Okay," said Saul. Sounds like fun!"
"The stork exercises may help," said Chelo. "But I still
think he needs a brace. At least at first."
We must weigh the advantages against the disadvantages,"
said Mari. "A long-leg brace would keep his knee straight. But
it could weaken the muscles he needs to strengthen. Since the
brace would keep his leg from bending back, he wouldn't have
to use his muscles to do it.
"On the other hand, we might try a short-leg brace that
holds his foot at almost a right angle. Then, to step flat he
will have to keep his knee nearly straight. It could help him
strengthen his behind-the-thigh muscles."
"Let's try it!" Everyone agreed, except Saul.

Chelo brought someone's old, lower-leg plastic brace and
showed it to Saul. "See how it will fit right around your leg.
It isn't heavy at all. Lift it! And no metal joints to get in
the way! What do you say? Do you want to try it?"
"I guess so," said Saul.
When the brace was made, they tested it. Saul said he liked
it. At first, when he tried hard, he could walk without
bending his knee back. But after a few days, his mother
complained that often he would walk, or even stand, with his
knee bent way back as before, and his toes in the air, like
this.


"I have an idea," said Chelo. "Why don't we let the heel
stick out behind the shoe. That way, when he steps, his weight
will come well forward of the back of his heel. This should
help bring his foot down and his knee forward."
They tried it, and most of the time (especially when he was
reminded) Saul walked without letting his knee bend back
much."

At home Saul's mother encouraged him to do his stork
exercises. As his muscles grew stronger, he began to walk
without bending his knee far back-even in active play!
071
WILL MY CHILD EVER BE ABLE TO WALK? "

This is often one of the first questions asked by the
parents of a disabled child. It is an important question.
However, we must help parents realize that other things in
life can be more important than walking (see
Page 93).
If the child whose legs are severely paralyzed by polio is
to walk, generally she will need at least 2 things:
1. fairly strong shoulders and arms for
crutch use
2. fairly straight legs (hips, knees, and
feet). (it is important to correct contractures so that the
legs are straight or nearly straight before trying to adapt
braces for walking.)
To evaluate a child's possibility for walking, always
test arm and shoulder strength:
Have her try to lift her body weight off the ground with
her arms, like this.
If she can easily lift up and down several times, she has a
GOOD chance of being able to walk using crutches.
If her arms and shoulders are so weak she cannot begin to
lift herself, her chances for crutch - walking are POOR.

If her shoulder and arm strength is FAIR, and the child can
almost lift herself, daily exercise lifting her weight like
this may increase strength enough to make crutch use possible.
Having the child lift herself while holding bar like this
will also help strengthen her hands and wrists for crutch use.
Pushing herself in a wheelchair or wheelboard (trolley) is
a practical way to strengthen shoulders, arms, and hands.

If the child cannot lift herself because of weak elbows,
put simple splints on her arms to see if she can lift herself
with these.

If she can lift herself with the elbow splints, maybe she
can use crutches that give elbow support.

If she is fat, she should lose weight.
This will make walking on weak limbs much easier.
Now check how straight the legs will go. (See
range-of-motion testing, Page 27.)

If the hips, knees, and feet can be placed in fairly
straight positions, chances for walking soon with braces are
good (if arm strength is good).
But if the child has much contracture of the hips, knees,
or feet, these will need to be straightened before she will be
able to walk.
For correction of contractures, see
Chapters 8 and
59.

Sometimes, if contractures are severe in one leg only, the
child can learn to walk on the other leg only, with crutches.
But it is best with both legs, whenever possible.
072
After checking arm strength and leg straightness, the next
thing to check is the strength in the ankles, knees,
and hips. This will help you decide if the child
needs braces, and what kind.
A child with a foot that hangs down (foot
drop), or flops to one side may be helped by
a below-knee brace of plastic or metal.
For foot drop, you can make a brace that lifts the foot
with a spring or rubber band. (See
Page 545.)
The kind of brace you choose will depend on various
factors, including cost, available skills and materials, and
what seems to work best for the particular child.
Advantages and disadvantages of different kinds of braces, and
how to make them, are discussed in
Chapter 58.
A child with a weak knee may need a
long-leg brace of plastic or metal.
Note:Not all children with no strength to
straighten the knee need long-leg braces:A child with
strong butt muscles may be able to walk without a brace.
If a child has a contracture and cannot walk with his
knee straight, correcting the contracture until his knee
bends very slightly backward may allow him to walk better. |

CAUTION: A stiff foot with a
moderate tiptoe contracture may help push the knee back,
just like a stiff brace. Correcting the contracture may
make walking more difficult or impossible, so that a brace
is needed where none was needed before. (See
Chapter 56.) |
073
A child with very weak hip muscles may
find his leg flops or twists about too much with a long-leg
brace.
He may need a brace with a hip band to help stabilize the
leg at the hip.

A child with weak body and back muscles,
who cannot hold up her body well, may need long-leg braces
attached to a body brace or body jacket.

Note: Often a child at first may
need a hip band or body jacket to help stabilize her for
walking. A few weeks or months later she may no longer need
it. Removing it may help the child gain more strength and
control. It is important to re-evaluate the child's
needs for bracing periodically.
| Take care to use no more bracing than is
needed. |

A child whose backbone is becoming seriously curved
may benefit from a body brace (or in severe cases, she may
need surgery).

If necessary, the body brace can be attached to long-leg
braces as shown above.
More information on spinal curve can be found in
Chapter 20. For
information on how to make body braces and jackets, see
Chapter 58.
074
PREVENTION OF POLIO

POLIO VACCINE, the best protection - IF it has been
kept cold continuously! |
 | Vaccinate babies with polio vaccine. Be
sure they get the vaccine 3 times by the time they are 8
months old. It is usually best to give the first polio
vaccination around 3 months of age. |
 | Vaccinate as many children as possible.
The vaccine given by mouth is alive. So, if most of the
children are vaccinated, the live vaccine will spread to
children who have not been vaccinated, and protect them
also. |
 | Try to Keep the live polio vaccine frozen
until shortly before it is used. For up to 3 months it can
be thawed and refrozen. But it must be kept cold or it will
spoil. |

 | Seek community help with vaccination
and in keeping vaccine cold. Sometimes vaccines do not reach
villages because health posts lack refrigeration. But often
store-keepers and a few families have refrigerators. Win
their interest and cooperation. |
 | To give best protection, vaccinate the child
when she does not have a fever or a cold or diarrhea.
But if by 6 months of age, the child still has not been
vaccinated, give her the polio vaccine even if she is a
little sick. However, there is a chance that the vaccine may
not work if it is given when the child is sick (with a virus
infection). Therefore, still try to give the complete series
of 3 vaccinations and one booster later, when the child is
not sick. |
It is estimated that in poor countries at least
one-third of vaccines are spoiled by the time they reach the
children. Therefore, even in children who
have been vaccinated, additional precautions are needed:

 | Breast feed your baby as long as
possible. Breast milk contains 'antibodies' that may help
protect against polio. (Babies rarely get polio before 8
months old because they still have their mothers'
antibodies. Breast feeding may make this protection last
longer.) |
 | Do not give injections of any medicine to babies
or children, except when absolutely necessary.
Irritation caused by injected medicine can turn a mild,
undiagnosed polio infection into paralysis. It is estimated
that today 1 out of 3 cases of paralysis from polio is
brought on by injections (see Page
19). |
 | Organize the people and help out in
popular campaigns to encourage vaccination, breast
feeding, and limited, sensible use of
injections. Community theater and puppet
shows are good ways to raise awareness on these
issues. See Chapter 48. |
075
PREVENTION of secondary problems
We have already discussed some ways to prevent new problems
or complications in a child with paralysis. In summary,
important measures include:
 | Prevent contractures and deformities.
Begin appropriate range-of-motion exercises
as soon as the paralysis appears. |
 | At the first sign of a joint contracture, do
stretching exercises 2 or 3 times a day- every day. |
| Stretching exercises work better if you
stretch the joint firmly and continuously for a few
moments,
|
instead of 'pumping' the limb back and
forth.

We emphasize this point because in many countries
parents are taught the pumping method - which does very
little good.
|
For more details, see "Contractures,"
Chapter 8.
 | Evaluate the child's needs regularly,
and change or adapt aids, braces, and exercises to
meet her changing needs. Too little or too much
bracing can hold the child back or create new problems. |

 | Be sure crutches do not press hard under the
arms; this can cause paralysis of the hands (see
Page 393). |
 | Try not to let the child's physical disability
hold back her overall physical, mental, and social
development. Provide opportunities for her to lead
an active life and take part in games, activities, school,
and work with other children.
PART 2 of this book
discusses ways to help the community meet the needs of
disabled children. |
OTHER PARTS OF THIS BOOK THAT MAY BE USEFUL
IN MEETING NEEDS OF A CHILD AFFECTED BY POLIO
* Especially important chapters are marked with a star:*
Physical examination,
Chapter 4
Measurement of contractures and progress,
Chapter 5
* Contractures, Chapter
8
Dislocated hips,
Chapter 18
Spinal curve, Chapter
20
* Range-of-motion and other exercises,
Chapter 42
Crutch use, wheelchair transfers, etc.,
Chapter 43
Community needs, social adjustment, growing up,
PART 2, especially
Chapters 47,
48,
52,
53
Making sure aids and procedures meet the child's needs,
Chapter 56
* Braces and calipers,
Chapter 58
* Correcting contractures,
Chapter 59
Correcting club feet,
Chapter 60
Special seating and wheelchairs, Chapters
64,
65,
66
* Aids for walking,
Chapter 63
For more information on polio, see References
Page 637.
|
076
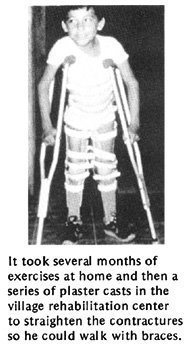
A BOY WITH POLIO BECOMES AN OUTSTANDING
HEALTH AND REHABILITATION WORKER
Marcelo Acevedo was disabled by polio. He and his
family lived in a village 2 days from the closest road.
Village health workers from Project Piaxtla helped Marcelo
get surgery for his knee contractures. After surgery he
got braces and went to school. Then they trained him as a
village health worker, and he returned to serve his
village.
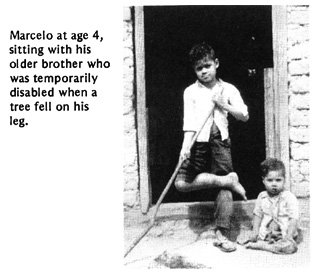
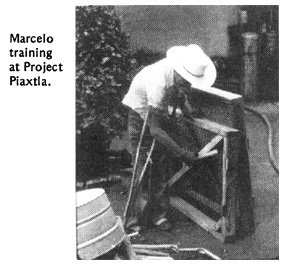
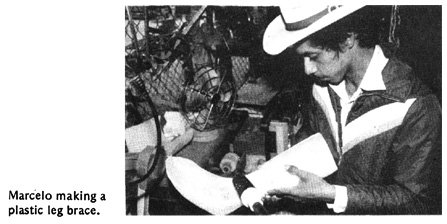
When PROJIMO was formed, Marcelo joined as a village
rehabilitation worker. He studied brace-making as an
apprentice in 2 brace shops in Mexico City.
Marcelo is now one of the leaders in PROJIMO, and has
gained the respect of the whole village. He has recently
married a village woman.
|