CHAPTER 25
Urine and Bowel Management
With Spinal Cord Injury and Spina Bifida
Most persons with spinal cord injury or spina bifida do not have normal bladder or bowel control (control for peeing and shitting). This loss of control can be inconvenient, embarrassing, and cause social and emotional difficulties. Also, the loss of control can cause skin problems and dangerous urinary infections. For these reasons, it is important to learn ways to stay clean, dry, and healthy. Most of the methods are not difficult, so children should be able to do it themselves. This will help them feel more self-reliant.
URINE MANAGEMENT
The main goals of urine management are:
- to prevent urinary infection, and
- self-care in staying as dry as possible.
Prevention of urinary infection is extremely important. Infections of the urinary system (bladder and kidneys) are very common in both spinal cord injury and spina bifida, and are one of the main causes of early death. Therefore, any method used for self-care or staying dry must also help prevent urinary infections. Make every effort to prevent germs from getting into the bladder. Keeping clean is essential. Also, it is important to empty the bladder regularly as completely as possible. If some urine stays in the bladder, bacteria will grow in it and cause infection.
| The ideal method of urine control empties the bladder completely and in a clean, regular, easy, and self-reliant way. |
Different methods work best for different persons-depending mostly on what 'type' of bladder a person has. We discuss this on the next page.
'Types' of bladder-in persons whose feeling and control have been partly or completely lost.
AUTOMATIC BLADDER: A person with paralysis whose legs have 'reflex spasms' (uncontrolled stiffening or jerking) usually also has reflex spasms in his bladder. As the bladder fills with urine, the wails of the bladder stretch and cause a reflex spasm. As the bladder squeezes, the muscles that hold back the urine relax, letting the urine flow out. This is called an 'automatic bladder' because it empties automatically when it gets full.
![]()
LIMP BLADDER (flaccid bladder): When a person's paralyzed legs are limp and do not have spasms, usually the bladder is also limp, or flaccid. No matter how much urine fills the bladder, it will not squeeze to empty. The bladder stretches until it cannot hold any more and the urine begins to drip out. The bladder does not completely empty this way. Some urine stays in the bladder, increasing the chance of infection.
The most simple methods of bladder management work well with an automatic bladder but do not work with a limp bladder. So try to figure out which type of bladder a child has.
For the first few days or weeks after the spinal cord has been injured, the bladder is almost always limp. Urine either drips out or does not come out at all. Then, as the 'spinal shock' wears off, persons with higher back injuries (above the 2nd lumbar vertebra, see Page 176) usually develop automatic bladders. In persons with lower back injuries, the bladder usually stays limp.
During the first weeks, usually a 'Foley catheter' is kept in the bladder all the time. However, after about 2 weeks, it is a good idea to test how the bladder works by removing the catheter and trying one of the methods described in this chapter. If the person is often wet, try another method for that type of bladder.
| A catheter is a flexible rubber tube used
for draining urine out of the bladder.
A 'Foley' catheter has a small balloon near the tip. This balloon is filled with water when it is inside the bladder, so that it can be left inside and will not slip out. Water is injected into the balloon here. Urine drains out here. For instructions on how to use a catheter, see Page 206. |
Methods for automatic bladder
1. TRIGGERING: This method usually causes the bladder-emptying reflex to work when the person is ready to pee. It can be done using a urinal, toilet, potty or jar. This is the first method to try because nothing is put into the bladder. It is easy, so a child can do it alone.

| Tap the lower belly (over the bladder) firmly with your hand for about 1 minute. Stop and wait for the urine to come. |
| Tap again. Repeat several times until no more urine f lows. |
If possible, once a week after triggering use a catheter to see how much urine is left. If there is less than a cupful (150 cc), continue the triggering program. It there is more than a cupful on several occasions, then the bladder is not emptying well enough. Try another method.

2. PERIODIC USE OF A CATHETER: This method allows the bladder to be emptied completely before becoming too full. Sometimes it can be used to prepare the body for triggering. Put a clean or sterile standard catheter into the bladder every 4 to 6 hours to empty the urine.
For instructions on how to put in a catheter, see the next page.
| CAUTION: If you drink more liquid than usual, put in the catheter more frequently to keep the bladder from stretching too much. |
Note: To reduce risk of urinary infections, regular frequent use of the catheter is more important than using a sterile catheter. It is a mistake to stop using the catheter only because you don't have a chance to boil it (for example, when traveling, or at school). Just wash out the catheter with clean drinkable water after use, and keep it in a clean jar or towel. (Do not go too long without catheterizing, and do not stop catheterizing altogether.) It is important for your bladder not to interrupt your program.
How to put in a catheter
Health workers and parents can easily be taught to put in a catheter. With a little practice, paraplegic and some quadriplegic children can also learn.
Note: The best catheter size is usually from #8 or #10 for a small child to #14 or #16 for a large child.
| Note: The great care with cleanliness shown here (boiling the catheter, wearing gloves) is important when using a fixed (Foley) catheter. However, for periodic use of a regular catheter, a clean rather than sterile technique is more practical (and therefore may be safer). Wash the catheter well with clean water after each use and keep it in a clean container. Wash your hands well before using it. See note on Page 205. |

1. If possible boil the catheter (and any syringe or instrument you may be using) for 15 minutes, or at least wash them well and keep them clean. |

2. Bathe well (at least daily). Wash well under foreskin or between vaginal lips and surrounding areas. |

3. Wash hands with soap. After washing touch only things that are sterile or very clean. |
4. Put very clean cloths under and around the area..
|
| 5. Put on sterile gloves-or rub hands well with alcohol or
surgical soap.
|
6. Cover the catheter with a lubricant (slippery cream)
1ike K- Y Jelly that dissolves in water (not oil or Vaseline).
|
| 7. Pull back foreskin or open the vaginal lips,
and wipe the urine opening with a sterile cotton soaked with surgical soap. |
8. Holding the lips open or the foreskin back, gently put
the catheter into the urine hole. Twist it as necessary but DO
NOT FORCE IT.
Hold the penis straight at this angle. |
| 9. Push the catheter in until urine starts coming out-
then 3 cm. more.
|
10A. If using a regular catheter, each time you pee tighten your stomach muscles or gently massage the lower belly to empty all urine. Then take out the catheter, wash it well, boil it, and store it in a clean jar or towel. |
| To avoid infections when using a catheter, it is important to be very clean and to use only a catheter that is sterile, boiled, or very clean. |
3. FOLEY CATHETER (fixed catheter): With this method, the catheter is left in all the time to drain the urine from the bladder continuously. A Foley is often used immediately after injury, and in some cases, for many months or years. The catheter connects to a collection bag that can be attached to the leg and worn under the clothes.
In many areas this is the easiest method because other supplies are difficult to get. However, a Foley can cause many problems, including:
| Bacteria can get into the bladder, causing a high risk of infection. | |
| Continuous bladder irritation can cause bladder stones to form. | |
| The catheter may cause a sore on the underside of the penis through which urine leaks. This may need surgery to correct. |
If you have tried other methods unsuccessfully or no other equipment is available, a Foley catheter may be the only choice. To prevent complications it is very important that it be used carefully:
| Always wash your hands well before touching the catheter. | |
| Clean the skin around the catheter with soap and water at least twice a day and after each bowel movement. | |
| Do not disconnect the collection bag except to empty and wash it. Wash it out with soap or bleach (Clorox) and water once a day. | |
| If the catheter must be clamped, use a sterile plug, never a glass ampule (small bottle). It may break and cause injury. | |
| Keep the collection bag below the level of the bladder to keep the urine from flowing back. | |
| Tape the catheter to the leg when in a wheelchair. Boys should tape the catheter on belly when lying down. | |
| Check regularly to make sure the urine is emptying and that the catheter is not plugged up. Avoid sharp bends or folds in the tubing. | |
| When turning, lifting, or moving the person, remember to move the bag too. Do not let it pull at the catheter or stay under the person. | |
| If the catheter gets plugged up, take it out, squirt boiled water through it, and put it back. Or use a new one. In emergencies, you can squirt a little (cool) boiled water back through the catheter while it is in place. Use a sterile or very clean syringe. |
4. CONDOM CATHETER: This is a practical method for men and boys who cannot control their urine. It can be used in combination with triggering, to avoid accidental wetting.
A condom catheter is a thin rubber bag that fits over the penis. It has a tube that connects to a collection bag. They come in different sizes.
If condom catheters are too costly or not available, a regular condom ('rubber', 'sheath', or ' prophylactic' for family planning) can be attached to the collection tube with a rubber band or tape.
Or a thin, very clean plastic bag can be used. Or, on a child, use the finger of a rubber glove (or a 'fingercot').
To hold the condom on the penis, a special very stretchy adhesive tape can be used as shown in this series of drawings.
| How to put on a condom using Con-stay
tape
Warning: Use only Con-stay or another easily stretchable adhesive tape. (Ordinary adhesive tape can stop blood flow when the penis swells.) |
|
1.  Cut off hair. |
2.
Pull back skin. |
3.
 Apply 'skin prep' (tincture of benzoin) to help condom stick to skin. |
4. Pull foreskin forward over head of penis.
|
5.
 Loosely wrap Con-stay tape around condom so it sticks to itself. |
6.
 Roll the condom back over the tape. |
7.
 Add a second strip of tape, ½ on the condom and ½ on the skin. |
8.
 Cut off the rubber rim. |
9.
 Connect condom to leg bag. |

One of the safest and cheapest ways to hold a condom on the penis is to cut a ring out of soft foam rubber. Pass the condom under the ring and turn it back over it.

The ring can be used again and again. So can the condoms if they are carefully washed.
IMPORTANT PRECAUTIONS FOR CONDOM USE:
| Be sure it is not too tight-it could stop blood flow and severely harm the penis. Avoid non-stretch tape. | |
| If the penis has erections (gets hard and bigger), try to put on the condom when it is big. | |
| Remove the condom once a day and wash the penis well. | |
| If possible, remove it at night. Use a bottle or urinal to catch the urine. | |
| Check the condom and penis often to be sure everything is all right. | |
| If the penis becomes injured, swollen, or looks sore, remove the condom until the penis is healthy. |
Methods for the limp bladder
If the person's bladder is limp (flaccid), it never empties by reflex. The bladder will constantly have urine sitting in it unless an effective emptying method is used.
Boys:
- Put in a regular catheter every 4 to 6 hours to empty the bladder. Between catheter use, the boy can put on a condom to catch any leaking urine, as described on Page 208.
- A Foley catheter can be used, but may lead to problems (see Page 207).
- Other alternatives include a surgical operation, which allows the urine to come out through a small opening on the belly into a bag. Or a special catheter is put into the bladder through a small hole in the lower belly.
Girls:
- They can use a Foley catheter. This is often the simplest method, but can lead to urinary infections.
- Or try an 'intermittent' (in and out) program, using a regular catheter every 4-6 hours. If there is leaking in between catheter times, use diapers, rags, or a thick sanitary pad to catch the urine. Change them often and wash often to protect the skin and prevent sores.
- The surgical procedures mentioned for boys can also be done in girls.
OTHER SUGGESTIONS FOR THE LIMP BLADDER-BOTH SEXES
The push method:
This method is recommended by many professionals, but it can cause problems. If the muscles do not relax to let the urine out, pushing on the bladder can force urine back into the kidneys-causing kidney infection and damage. Therefore, the push method should only be used if the urine comes out easily with gentle pressure-or if there is no other way possible. | |||
| With boys with a limp bladder, the condom method can be used. But it is best to also use a regular catheter at least 3 times a day. This is because the bladder does not empty completely, which makes infection more likely. |
URINARY INFECTIONS
Persons with spinal cord injury or spina bifida have a high risk of urinary (bladder) infections, for the reasons we have discussed. Long-term or untreated infections and kidney problems are a common cause of early death. Preventive measures are essential (see the bottom of the next page); but even when precautions are taken, some urinary infections are still likely to happen. Therefore, it is very important to recognize the signs and provide effective treatment.
Signs
When a person who has normal feeling has a urine infection, it burns when he pees. The person with spinal cord damage may not feel this burning and therefore has to use other signs to know when he has an infection. He may learn to recognize certain unpleasant feelings, or may only know that he does not feel as healthy as usual. Parents and health workers should learn to listen to the child and be aware of changes in behavior or other signs that might mean that he has an infection.
Possible urinary signs
| cloudy urine, possibly with pieces of mucus, pus, or blood specks | |
| dark or red urine | |
| strong or bad smelling urine | |
| increased bladder spasms (cramps) | |
| increased wetting or changes in bladder function | |
| pain in the mid-back (kidneys) or side (urine tubes) |
Possible other signs
| body aches | |
| general discomfort | |
| increased muscle spasms | |
| fever | |
| dysreflexia (headache, goosebumps when sweating, high blood pressure, see Page 187.) |
Treatment
At t he first signs of infection, drink even more water than usual. Antibiotics (medicines that fight bacteria) may also be necessary. But avoid frequent use of antibiotics because they may become less effective (bacteria may become resistant).
If a person has had urinary infections before, he can start with the last medicine that was effective. If not ...
| Start with one of the medicines in Group 1 on the next page. If after 2 days the person is still getting worse, try another medicine in Group 1. | |
| If that does not help, try one of the medicines in Group 2. | |
| If none of the medicines of Group 2 help, take the person to a medical laboratory for a 'culture' and 'sensitivity test' of the urine. | |
| If that is not possible, try a medicine in Group 3. If possible, consult a specialist in urinary problems. |
If a medicine seems to help, continue taking it for at least a week, or for 4 days after the last signs have disappeared. Do not change from one medicine to another unless the medicine is not working or causes serious side effects.
CAUTION: Many of these medicines sometimes cause serious side effects. Find out about their risks and precautions before using them.
* The medicines marked with a star (*) can cause kidney damage unless the person drinks lots of water.
Be sure to give the medication in the correct dosage.
TREATMENT FOR URINARY INFECTIONS
| Medical name (and common brand) | Age | Dose | Repeat the dose | |
| Group 1 | A.* Sulfisoxazole (Gantrisin) |
up to 5 years 5 to 10 years over 10 years |
500 mg. 750 mg. 1000 mg. |
4 times a day |
| B. Nitrofurantoin (Furadantin, Macrodantin) | up to 5 years over 6 years | 25mg. 50mg. |
4 times a day | |
| Group 2 | A. Ampicillin (many brands) | up to 4 years 4 to 8 years over 8 years |
125mg. 250mg. 500mg |
4 times a day |
| Caution: Do not use for persons allergic to penicillin | ||||
| B.* Sulfamethoxazole 400 mg. with trimethoprim 80 mg. (Bactrim or Septra) |
up to 4 years 4 to 9 years 9 to 12 years over 12 years |
1/2 tablet 1 tablet 1 1/2 tablets 2 tablets |
2 times a day | |
| Note:
This medicine also comes in double strength
(Bactrim DS and Septra DS). Adjust doses if using double strength. |
||||
| C. Cephalexin (Keflex) or a similar 'cephalosporin' | up to 5 years over 5 years |
125mg. 250mg. |
4 times a day | |
| Group 3 | A. Carbenicillin (Geocillin) | up to 6 years 6 to 10 years over 10 years |
1/4 tablet 1/2 tablet 1 tablet (382mg.) |
4 times a day |
| Note: Take 1 hour before or 2 hours after eating. | ||||
| B. Tetracycline (many brands) | over 8 years | 500mg. | 4 times a day | |
| Caution: Do not give to children under 8 years, or to women who are pregnant or breast feeding. If possible, avoid taking milk products with tetracycline. | ||||
| All persons with a urinary infection should always drink lots of water while they are taking medicine. After the infection is gone, continue drinking lots of water, and take all preventive measures. | ||||
PREVENTION OF URINARY INFECTIONS

| Drink lots of liquid-adults, at least 2 liters (8 glasses) a day. | |
| Eat apples, grapes, or cranberries-or
drink their juices-or take vitamin C tablets
to make urine more acid. Bacteria grow with
more difficulty in acid urine. (Note: Orange or lemon juice and other citrus fruits and juices do not work! They make the urine less acid.) | |
| Keep hands, catheter, and collection bags very clean before, during, and after your bladder program. | |
| Do not lie in bed all day. Stay active. | |
| Do not clamp the Foley catheter or plug it with anything - unless absolutely necessary - then use a sterile plug. | |
| Stick to your bladder program. Do not allow urine to sit in bladder | |
| Do not let the catheter get bent or twisted so that urine cannot come out. | |
| If using a standard catheter periodically, be sure to put it in regularly, at least every 4 to 6 hours. To prevent infections, frequency of catheter use is even more important than cleanliness. It is safer to put in the catheter without boiling it, than not to put it in. If infections are common, catheterize more often. |
BOWEL MANAGEMENT IN SPINAL CORD INJURY AND SPINA BIFIDA
When there is damage to the spinal cord, almost always a person loses control over when he will have a bowel movement (pass stool or shit). This makes it hard to stay clean, which can be inconvenient or embarrassing. Although he can never get back complete control over the muscles that hold in or push out the stool, a person can learn to help the stool come out, with assistance, at certain times of day. This kind of 'bowel program' can greatly increase the person's self-confidence and freedom for school, work, and social activities.
Persons with spinal cord damage also often have problems with constipation, or the formation of hard stools that may wait days before coming out. Some constipation can be an advantage when a person lacks bowel control. But sometimes it can lead to serious problems, such as impaction (see Page 214) or dysreflexia (see Page 187). It is therefore important to prevent serious constipation:
| Drink lots of water. | |
| Eat foods high in fiber (such as bran, whole grain cereals, fruits, vegetables, cassava, beans, nuts). | |
| Stick to a scheduled bowel program. | |
| Keep active. |
Planning a bowel program
Any bowel program will work better if you:
| Do the program every day (or every other day) and at the same hour. Do it even if the person has had an accidental bowel movement shortly before, or has diarrhea. |
| Do the bowel program at the same time of day that the person usually had bowel movements before his injury. Often the bowels move best after a meal or a hot drink. | |
| If possible, do the program on a toilet or pot. The bowels work better sitting than lying. | |
| Be patient. The bowels sometimes take days or weeks to change their pattern. |
Types of bowel
Different persons require different types of bowel programs, depending on whether their bowels are 'automatic', 'limp', or 'pull back'.
| Automatic bowel usually occurs in persons who have muscle spasms in their legs, and an 'automatic bladder'. The muscle or 'sphincter' in the anus (asshole) stays shut until there is a stimulation in the bowel to make it open, so that the stool can come out. An automatic bowel will 'move' in response to a suppository or stimulation by a finger. | |
| Limp or 'flaccid' bowel usually occurs in persons with low spinal cord damage who have limp (not spastic) legs and bladder. The sphincter muscle in the anus is also limp. So the person tends to 'ooze' or 'dribble' shit. A limp bowel does not respond to finger stimulation. | |
| A bowel that pulls back is neither automatic nor limp. When you put a finger up the anus, you can feel the stool move back up instead of coming out. |
PROGRAM FOR AN AUTOMATIC BOWEL
| Start with a suppository if available. With a finger covered with a glove or plastic bag, and then oil, push the suppository about 2 cm. (1 in.) up the anus. Do not push it into the stool, but push it against the wall of the bowel. (Or try the program without a suppository; usually finger stimulation is enough.) | |
| Wait 5 or 10 minutes. Then help the person sit on a toilet or pot. If he cannot sit, have him lie on his left side (on top of old paper). | |
| Put an oiled finger into the anus about 2 cm. Gently move the finger in circles for about 1 minute, until the anus relaxes and the stool pushes out. | |
| Repeat the finger action 3 or 4 times, or until no more stool is felt. | |
| Clean the butt and anus well and wash your hands. |
SUPPLIES NEEDED
|
PROGRAM FOR A LIMP BOWEL
Since the bowel does not push, the stool must be taken out with a finger. It is best done after each meal, or at least once a day.
| If possible, do it sitting on a toilet or pot, or lying on your left side. | |
| With a gloved and oiled finger, remove as much stool as you can. | |
| Since a limp bowel tends to ooze stool, eat foods that make the stool firm or slightly constipated (not much stool-loosening foods). |
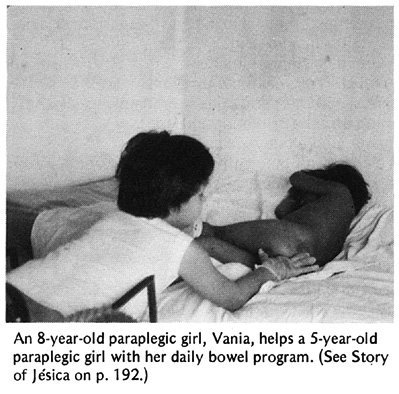
Children can learn to do their own 'bowel program'. (See Page 212.)
PROGRAM FOR A BOWEL THAT PULLS BACK
For this kind of bowel, the bowel programs already described usually do not work. Finger stimulation makes the bowel act in the opposite direction, and pull the stool back in. The person will have 'accidents' during the day. Often it works better to,
| First, put some anesthetic jelly (such as Xylocaine) up the anus. If you cannot get the jelly, you can mix some liquid injectable Xylocaine (lidocaine) with Vaseline or any other jelly. | |
| Wait several minutes. Then do the automatic bowel program. |
OTHER IMPORTANT POINTS
| Do not use enemas or strong laxatives regularly. They stretch the bowel, injure its muscles, and make following a regular program more difficult. A mild laxative may be taken occasionally, when needed. However, drinking more liquid and eating food high in fiber is usually enough. | |
| If there is bright red blood in the stool, probably a blood vessel was torn during the program. Be more gentle! If there is dark, old blood and the stools are black and tar-like, seek medical advice. | |
| A small amount of liquid stool (diarrhea) may be a sign of 'impaction' (a ball of hard stool stuck in the gut). Only liquid can leak around it. Do not give medicine to stop diarrhea; this could make the impaction worse. Try to get it out with a finger. |
| A bowel program may at first seem difficult and messy. But it soon becomes an easy habit. It is very important both for the person's health and his social well-being. Start now, do it regularly at the same hour, and DO NOT MISS A DAY. |